Dashboard
The ANZHFR has developed this Dashboard for patients, families, friends, and carers. It uses data from Australian hospitals submitted to the Hip Fracture Registry.
How does the ANZHFR help to improve care?
- Each time a person is admitted to hospital with a broken hip, staff at the hospital collect the same information for each person.
- The information is then entered into a secure system in Australia for Australian hospitals and a secure system in New Zealand for New Zealand hospitals.
- The staff at the ANZHFR then study the data and check it is complete and as correct as possible.
- The ANZHFR uses the data to create reports which show each hospital and how they compare to all the others.
- Hospitals use their data and the publicly available reports to review the care they provide and make improvements where the data tells them improvement is needed.

Each year there are more than 20,000 older people who break their hip. Most people break their hip from a slip, trip or fall.
In 2023, the Hip Fracture Registry recorded 14,066 people in Australia with a new hip fracture. They were admitted to 79 different hospitals.
All the data presented below comes from the Australian Hip Fracture Registry and is from the 2023 year.
To get an idea of the age of people when they injure their hip, all the data has been grouped by age. The bigger the circle the more people in this age group have broken their hip and been admitted to hospital during the year.
This Dashboard tells you what treatment is recommended when a person has been taken to hospital with a broken hip. Watch this short 5-minute video to see what care should be provided.
After watching the video, scroll down the page to see data from the ANZHFR about the national quality statements.
Use the filter to show data for someone like you.
= all ages
= all abilities
= all residences
= all states
The Injury
To help you understand the path from injury to rehabilitation, lets meet Margaret.
Margaret lives at home with John and is usually active, walking for exercise each day and volunteering at the local library.

Unfortunately, Margaret tripped on a carpet at home and hurt her hip.
Not being able to get up, John called an ambulance to take Margaret to the hospital.

Care when arriving at hospital

The ambulance took Margaret to the Emergency Department (ED).
Although it is busy, the staff work to get her to a bed in a suitable a ward within 4 hours of arriving at the ED.
She had x-rays and lots of other tests, including tests of her memory and thinking. This is called a ‘cognitive assessment’.
Time in the Emergency Department
What do I need to know?
Most people with a broken hip will spend time in the ED before being admitted into the hospital.
The ED is where the staff will arrange for x-rays and other tests to be taken to diagnose a broken hip.
Information about what to expect while in hospital should be provided and tests organised so that admission to the hospital happens as soon as possible.
Most people with a broken hip will spend time in the Emergency Department before being admitted into the hospital.
The ED is is a busy ward but they are the best place to assess and diagnose injuries.
They allow for early decisions to be made about the best treatment for a broken hip.
Let the staff know if you are uncomfortable in any way.
Share anything you think is important, especially any other medical conditions as these may affect any treatment provided.
Answer any questions asked by the staff, even if the questions are repeated.
Preoperative cognitive assessment
What do I need to know?
The staff will ask questions about your memory, thinking and communication because older people can have problems with these especially after an injury.
The staff may call this a ‘cognitive assessment’ and it should be repeated throughout the stay in hospital.
Memory problems can be an existing health conditionand can affect recovery from a broken hip.
Problems with memory, thinking and communication put a person at risk of being confused while in hospital. This confusion is called delirium.
It will slow recovery and increase a person’s risk of getting a complication while in hospital.
Assessing memory and thinking allows the staff to put in place strategies to reduce the risk of confusion while in hospital.
Ask the doctors and nurses about what the assessment of memory, thinking and communication showed.
Ask them what strategies are recommended be reduce the risk of confusion.
While in hospital, let the staff know about any changes to your usual memory, thinking and communication. Those who know you well may be the first to notice any changes.

Managing pain in hospital
When Margaret first arrived in the ED, she was asked about her pain within the first 30 minutes and was given pain relief because it is needed.
Margaret was given a ‘nerve block’ which numbed her leg. Managing Margaret’s pain early means that moving for x-rays and nursing care is not too uncomfortable.
For the whole time she was in hospital, Margaret was asked whether she was comfortable. This is important because avoiding discomfort and pain helps to avoid other complications.
Keeping people out of pain is important. You should be asked about your pain within 30 minutes of arriving in the ED and asked regularly for the whole time you are in hospital.
Most people need painkillers while waiting for their operation. Paracetamol is commonly used but stronger painkillers are frequently needed.
The medicine provided should be enough so that you are comfortable moving for x-rays and nursing care.
Staying relatively comfortable while waiting for an operation means you are less likely to have an episode of confusion caused by the pain.
Using medicine to stay as comfortable as possible will also help you to participate in your rehabilitation after the operation.
Even though you have been told you have a broken hip, it is best to avoid being really uncomfortable at any time.
If you are feeling uncomfortable for any reason, tell the doctors or nurses.
Ask for additional medicine so you can move comfortably in the bed and for any x-rays, scans and exercises that are needed.

Caring for you in hospital


The x-ray showed Margaret had broken her hip, so she was admitted to hospital and plans were made for treating her broken hip.


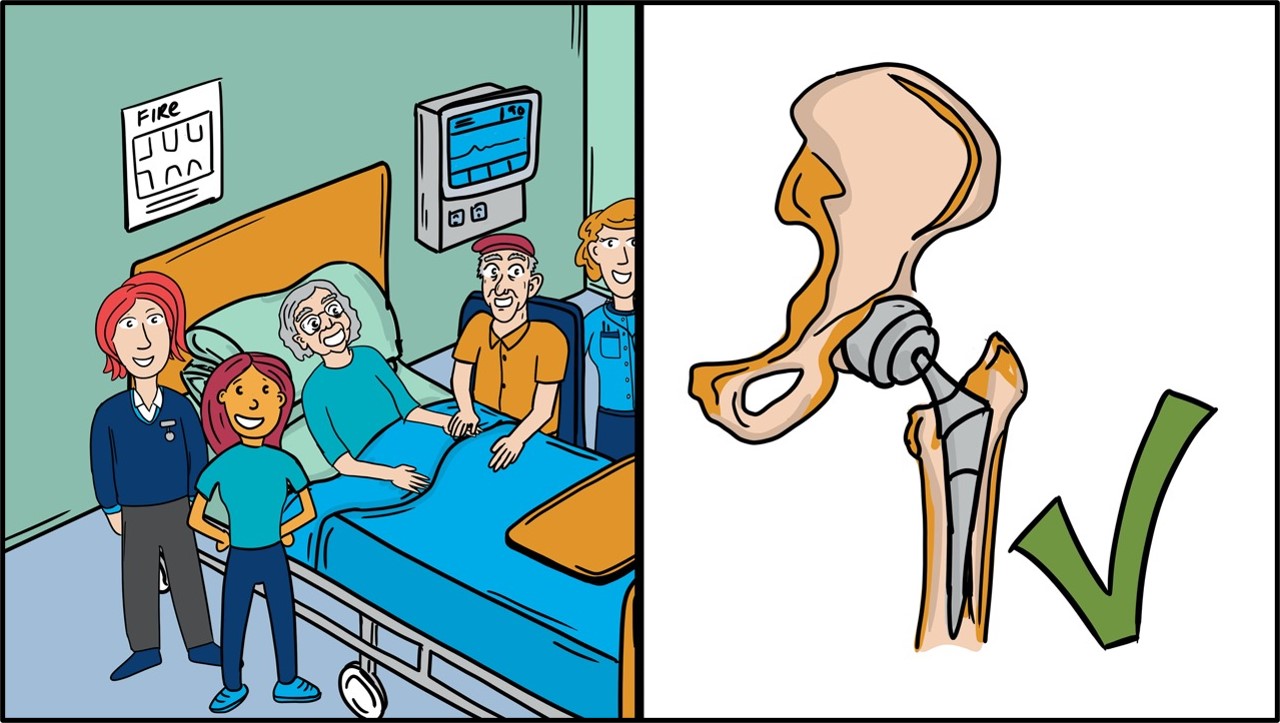
In the hospital, Margaret was looked after by a multidisciplinary team of doctors, nurses and allied health professionals.
To help with planning the right treatment, Margaret was asked lots of questions by the orthopaedic surgeon, anaesthetist, and a doctor or nurse with special knowledge of the medical conditions of older people.
These questions were about Margaret’s other medical conditions, her usual day-to-day activities, as well as her memory and thinking.
This helped the team understand her goals of treatment.
Preoperative medical assessment
What do I need to know?
The care provided in hospital is best when shared between health professionals with different expertise. Most commonly, three different specialist doctors lead the team.
These doctors are an orthopaedic surgeon, an anaesthetist, and a medical doctor who specialises in the care of older people.
These medical doctors are called Geriatricians. If a Geriatrician is not available, a general Physician, or a General Practitioner, or a specialist Nurse may be involved.
There will be other clinicians at the hospital who will also be involved in care. All the different clinicians looking after a person with a broken hip are called a ‘multidisciplinary team’.
Older people with a broken hip often have other health conditions that are made worse by the injury to their hip. It has been shown that the best care and the best outcomes for patients is provided by a team.
The benefits of shared care and a partnership between orthopaedic surgeons, anaesthetists, and geriatricians include fewer complications (like chest infections, pressure injuries and confusion) and improved physical recovery.
Be aware that you will meet lots of different doctors, nurses and other health professionals while you are in hospital.
Ask any questions you may have about your care and expected recovery until you are happy with what is being done and why. The treatment you receive for a broken hip will be best if you are involved in the decisions about treatment.
Share your other medical conditions with the physician doctors. Decide what your goals of treatment are and tell the multidisciplinary team.

Fixing the broken bone
The doctors recommended to Margaret an operation to fix her broken hip.
After considering the doctor’s recommendation and discussing it with John, Margaret agreed to have an operation to fix her broken hip.
Plans were made to do the operation within 48 hours of arriving at hospital because this helps reduce the risk of complications and also helps Margaret to start her recovery.
Surgery within 48 hours
What do I need to know?
Most people need an operation to fix the broken bone.
If an operation is agreedby you and your doctors, the hospital should be organised so that you are able to have the operation to fix the broken hip within 48 hours of arriving at hospital.
This 48-hour timeframe includes people who are transferred to another hospital for their operation. The 48 hours does not include people where a medical problem that needs to be treated before an operation.
If a delay is necessary then the doctors should explain why the surgery is delayed and you should be given the opportunity to ask questions.
For some people a decision is made that surgery is not the best option.
Early surgery improves the chance of a meaningful recovery. It reduces the chance of complications like pressure injuries and pneumonia.
The operation will allow you to stand and step the next day. This starts your rehabilitation and is an important achievement for beginning recovery.
Ask the doctors when your surgery will be done. If it is delayed, make sure you understand the explanation for the delay.
Ask the surgeon whether you will be able to stand on the operated leg the next day. Ask questions about the surgery until you are happy with what is being done and why.

Walking and rehabilitation after surgery
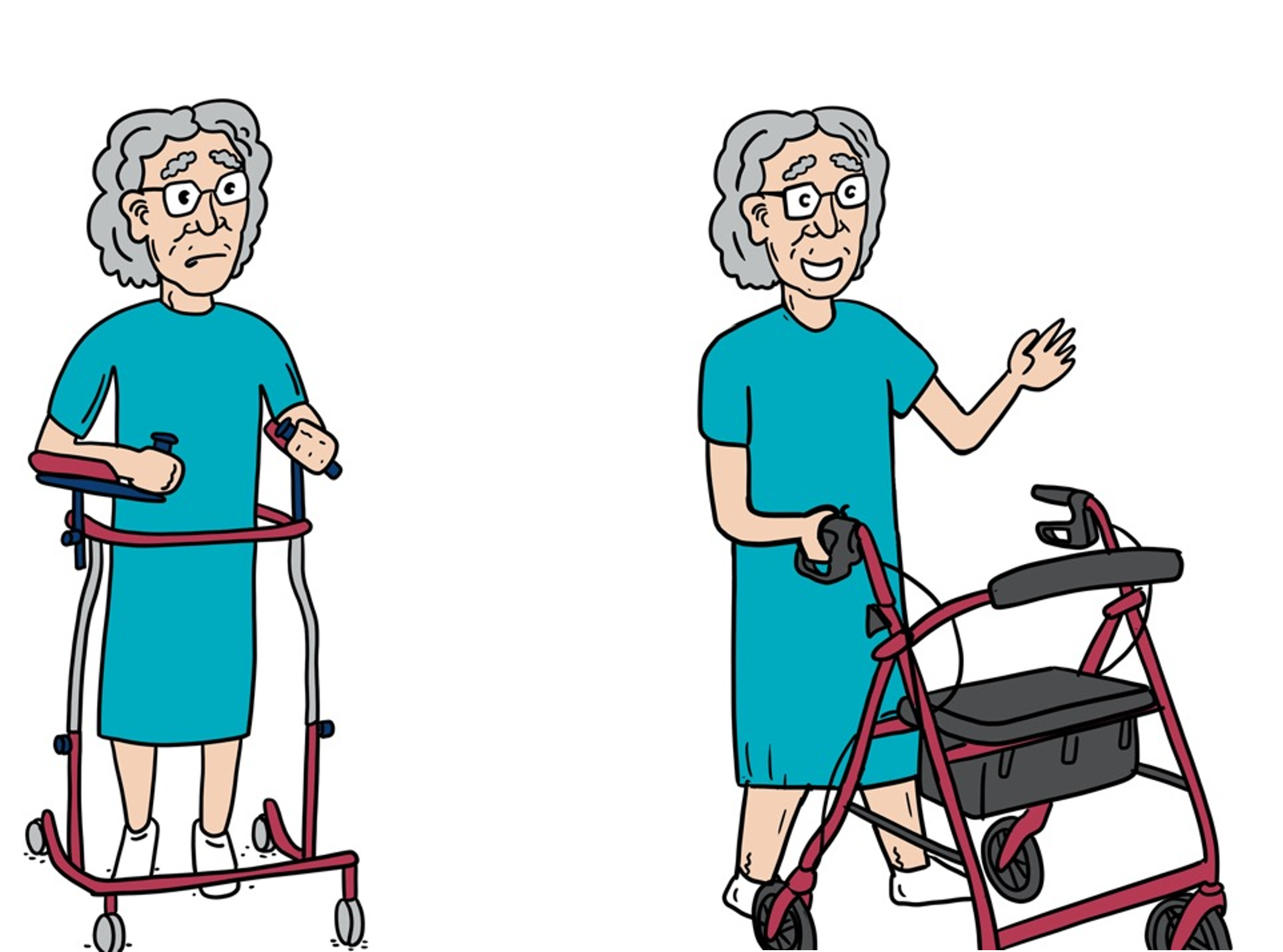
The day after the operation, Margaret was given an opportunity to stand up and take some steps.
Research has shown that people who are able to stand and step the day after surgery have better mobility and more independence, even after 12 months.
Getting up can be scary and very hard but with the support of the multidisciplinary team, and her family and friends, Margaret felt able to try to get up the day after the operation.
Postoperative weight bearing
First day walking
What do I need to know?
In most cases, the operation is done to allow standing and walking withour restriction from the first day after surgery.
There may be some discomfort or weakness when you first get out of bed. This is common. The physiotherapists and nurses are the team members that will be there to help and you will not be expected to do this on your own.
Early walking after hip fracture surgery improves movement and activity and decreases the chance of complications like pneumonia and pressure injuries.
It has been shown that the earlier people stand up and step the earlier they recover. This link between early activity and recovery continues from hospital all the way to 12 months later.
Expect to have someone ask you to get out of bed the day after your surgery. If you are worried about getting up out of bed, let the health professionals know.
If you would like family or a friend to be there when you get up for the first time, let them know the day after the operation is the day.

Preventing another broken bone
Margaret was told by the doctors that having a broken hip increased her risk of another broken bone in the future.
Even though she was usually active, she would really like to know what else could be done to reduce the chance of another break because she doesn’t want to go through this again.
The multidisciplinary team recommend eating foods high in calcium and vitamin D, doing strength and balance exercises, and talking to the doctor about bone strengthening medicine.
Bone medication at discharge
What do I need to know?
Assessing the things that may increase the risk of another fall allows them to be identified and modidified where possible.
Some risks can’t be changed, like age, but other risks like some medicines, vision problems, or lack of strength and balance can be changed with targeted strategies. These strategies can change the environment, like installing rails at home, or removing cords or mats that are a trip hazard. Or be strategies for you, like exercise classes or checking your vision and glasses.
Falling and breaking a hip means that the bones are not as strong as they need to be. There are medicines for strengthening bones that have been shown to decrease the risk of another break. The doctors or nurses should discuss these medicines with you while you are in hospital.
Improving nutrition, scussing bone medicines, changing fall risks, and improving strength and balance give the best chance of a full recovery. Making some simple changes may decreases the chance of another broken bone.
What do I need to do?
While you are in hospital talk to the health professionals about what can be done to decrease the risks of another fall. Discuss exercise, nutrition, bone medicines and the home environment.
Make sure a prevention plan is made with you after leaving hospital. This plan should be developed with you not about you.
Follow up with your family doctor in the first three months after leaving hospital. Discuss what can be done to decrease the risk of another broken bone.

Leaving hospital
Each day, Margaret walked a little bit further and gained a little bit more confidence but she was apprehensive about how she would manage at home.
Margaret and John had many conversations with the different health professionals until they were happy that the plan for her ongoing recovery
was just right for her. Margaret wanted the best chance of getting back to the things she enjoyed.
The recommendations from the multidisciplinary team and a plan for after leaving hospital are written down in an individualised care plan. A copy is given to Margaret and also sent to her family doctor.
Margaret is now ready to start the next part of her recovery.
Before you leave the hospital the clinical team (a doctor, nurse, physio or occupational therapist) should discuss with you how to continue your recovery at home. This should be written down and include your goals for after you leave the hospital. These goals should be developed from what is important to you.
Thess discussions should also make sure you know about any changes to your medicines, any equipment that is needed at home, where your rehabilitation will take place, any appointments that have been made, and what to expect from your recovery.
All of the decisions made from these discussions should be documented in what is called ‘An Individual Care Plan’. It should be provided to you before you leave so there is time to discuss it if there are any questions.
It is important to know that recovery continues after leaving hospital. Having a plan can help with what you need to know and who you need to see.
What do I need to do?Make sure you leave hospital with a documented ‘Individual Care Plan’ that provides enough information for you to know what your recovery after hospital should include. The care plan should include medicines, rehabilitation, equipment, appointments, wound care, graded activities, and community services.